Beta blockers: A central role in cardiac disorders
by egpat 22-08-2017
Beta blockers are one of the most widely prescribed drugs in various cardiovascular disorders. These drugs can be easily identified by the suffix “-olol”. For example, propranolol, timolol, metoprolol, nadolol etc. We can easily relate the suffix of beta blockers with their structure as all these drugs are chemically derived from aryloxypropanolamines.
See 40 suffixes of drugs for complete list of drugs and their unique suffixes.
Where the beta receptors located?
Before going to discuss the role of beta blockers, we should know the location and role of beta receptors in our physiological system.
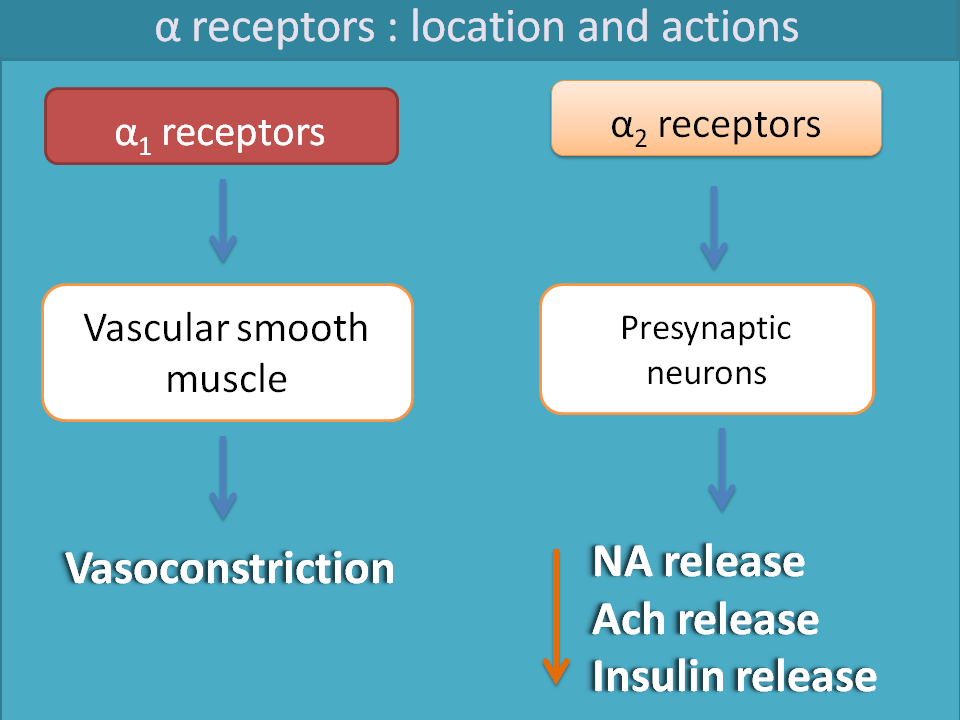
It is a well known fact that sympathetic system acts mainly by two receptors viz. alpha receptors and beta receptors. Alpha receptors are further categorised into α1 and α2 . Among these, α1 receptors are mainly present on vascular smooth muscle leading to vasoconstriction. α2 receptors are auto inhibitory in nature mainly present within the CNS.
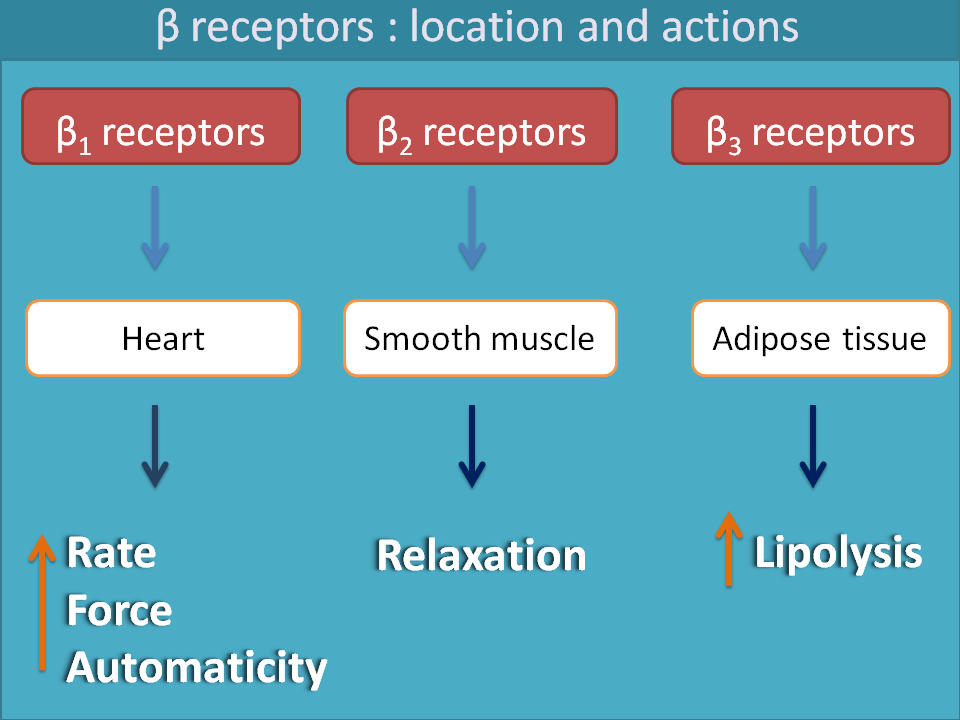
Similarly β1, β2 and β3 receptors are located on heart, smooth muscle and adipose tissue respectively. β1 receptors stimulate the heart increasing both rate and force of contraction of the heart. β2 receptors are responsible for relaxation of various smooth muscles like bronchial smooth muscle, GI smooth muscle, bladder, uterine and even vascular smooth muscle.β3 receptors play role in lipolysis.
As our current topic focuses on beta receptors, we extend our further discussion on them.
What is the role of beta receptors?
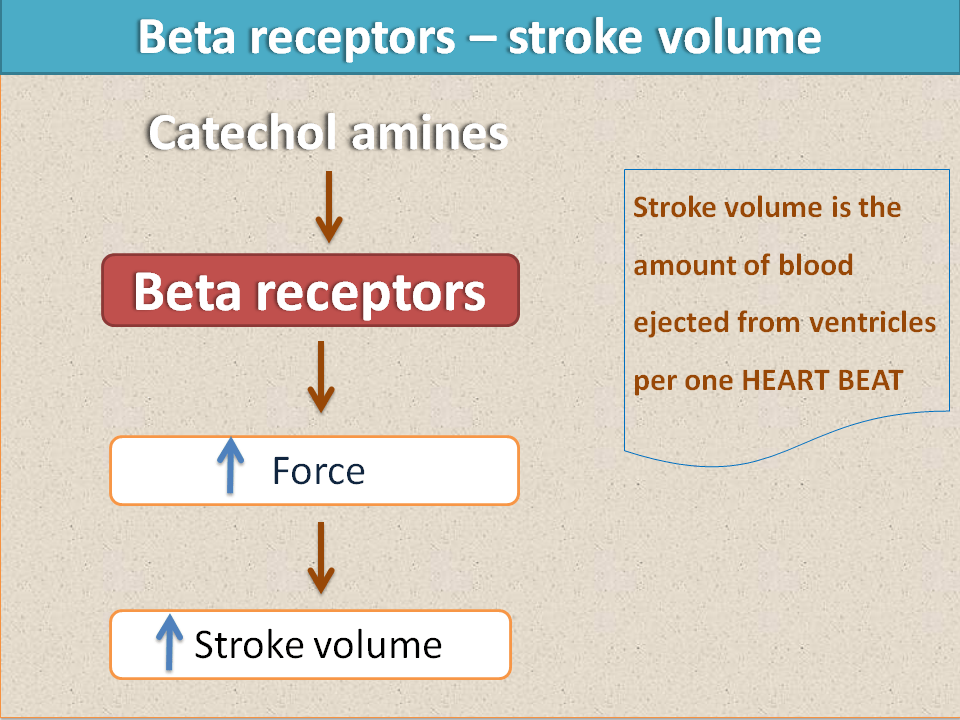
We already discussed that three types of beta receptors are present in sympathetic system. Beta 1 receptors are mainly present on the heart and responsible for cardiac stimulation. They increase rate and force of contraction of the heart. So, as the force increases, the net volume of the blood pumped by the heart per each heart beat i.e. stroke volume increases.
As the rate of contraction increases, the net amount of the blood ejected per one minute i.e. cardiac output also increases.
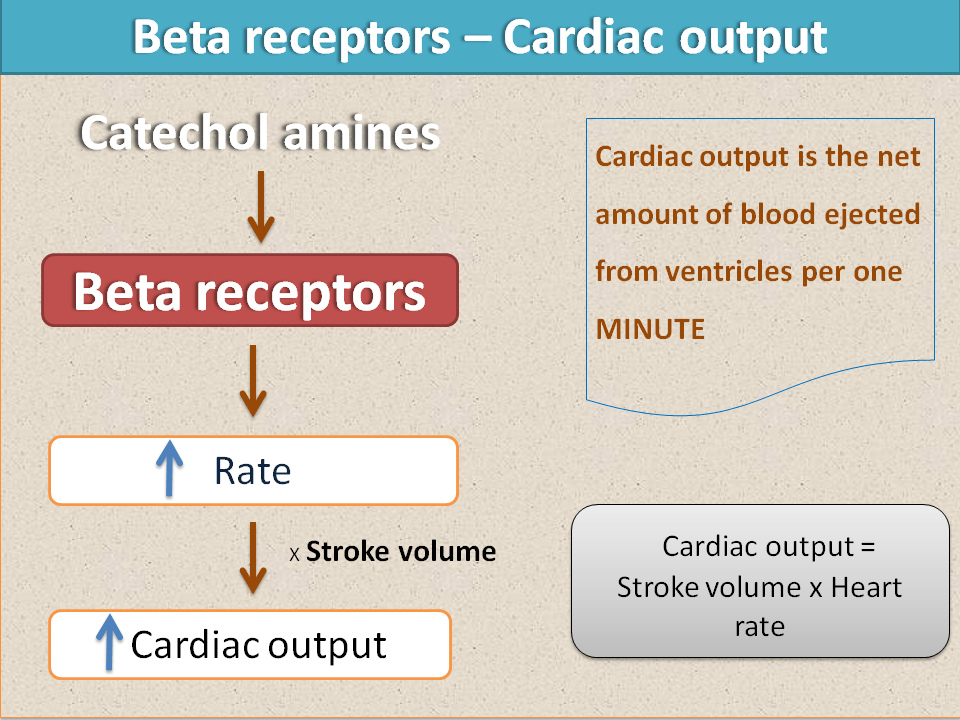
So, finally beta receptors have a great effect in increasing cardiac output. This results in enhanced blood supply to all the systemic organs supplying more energy. That’s why under stressful conditions sympathetic system is activated to increase blood supply to vital organs.
That’s fine.Then what’s wrong with beta receptors? Why should we use beta blockers?
Yes, there is no doubt that beta receptors improve the performance of vital organs by increasing blood supply but this is not without adverse effects. As cardiac output increases, cardiac work also increases requiring more oxygen to heart. So, cardiac oxygen consumption increases and as the condition persists for longer time cardiac efficiency decreases.
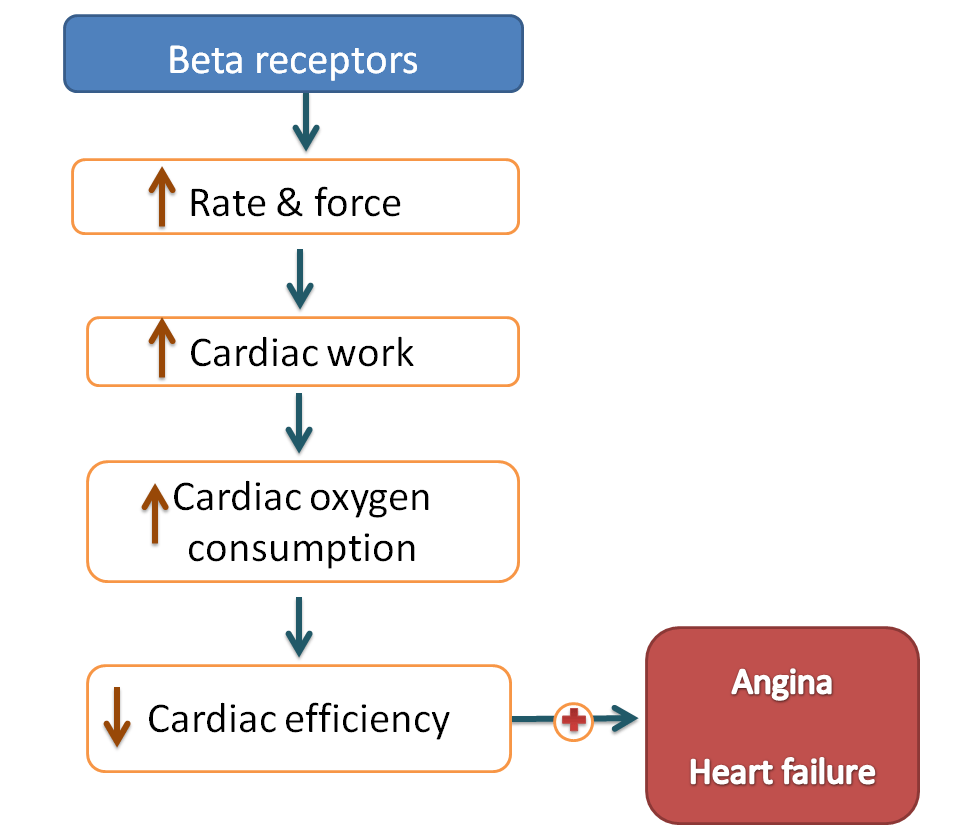
In summary, beta receptors increase the cardiac output enhancing the performance of vital organs but when they are activated persistently they decrease cardiac efficiency finally leading to cardiac failure.
When we need beta blockers?
Let’s have more clarification. Suppose, a person is under an exercise or stressful conditions, for example, he/she is on running. Now the person requires more energy to run, so, sympathetic system is activated to supply more energy to skeletal muscle. So, in that person heart rate increases, force of contraction and cardiac output increases. This is a temporary condition and whenever the running is completed, sympathetic system is slowly deactivated bringing back to the normal levels. Now heart rate and cardiac output all are normal. This is the homeostasis that is maintained by parasympathetic system working along with sympathetic system.
Now let’s see a pathological condition. Suppose a patient was attacked by angina. The patient got severe pain in the heart which stimulates sympathetic system. This enhanced sympathetic discharge increases cardiac oxygen consumption further deteriorating the angina condition. So in this patient, we should use beta blockers in order to prevent sympathetic activation and its deleterious effects aggravating the disorder.
Beta receptor activation is sometimes essential but when it is persistent it may be pathological.
❞Cardiovascular disorders like hypertension, angina, and arrhythmias are associated with persistent increase in sympathetic system requiring the use of beta blockers.
Why beta blockers are more important over alpha blockers?
Just above, we have seen that sympathetic activation should be controlled in few of the cardiovascular diseases to prevent further deterioration. But which receptors should be blocked whether alpha or beta receptors?
Right, we will come to the point. Sympathetic discharge acts both on alpha and beta receptors but activation of alpha receptors leads to vasoconstriction increasing blood pressure. So when alpha blockers are used they decrease only blood pressure but do not block all cardiac actions of catechol amines. Moreover, alpha blockers are direct vasodilators that produce postural hypotension and reflex tachycardia hence preferred only in treatment of resistant hypertension.
On the other hand, beta blockers inhibit the action of catecholamines mainly on the heart thereby inhibit all cardiac events associated.
Various categories of beta blockers
Beta blockers can be categorised mainly into five categories .
- Non-selective beta blockers
- Selective beta blockers
- Beta blockers with partial agonist activity
- Beta blockers with vasodilatory actions
- Beta blockers with alpha blocking activity
For complete classification see adrenergic antagonists.
Role of beta blockers in few disorders
So, now let’s see the role of beta blockers in cardiovascular disorders.
Hypertension
Let’s start our discussion with the case of hypertension. The elevated blood pressure in hypertension is due to various factors among these sympathetic activation shows its own mark. When sympathetic system is activated, the rate and force of contraction of the heart increase leading to increase in the cardiac output. This can result in increased after load, putting more pressure on the blood vessels.

Sympathetic system also increases systemic vasoconstriction of course this is through α1 receptors leading to direct raise in the blood pressure.
So, two important drug targets that act on sympathetic system include α blockers and β blockers.
α1 blockers are the vasodilators that directly act on vascular smooth muscle and decrease blood pressure. Due to their direct action on vascular smooth muscle, they may be associated with side effects like postural hypotension and reflex actions like tachycardia.
Since here our discussion is more focussed on beta blockers, we will extend our discussion on them. Beta blockers like propranolol, nadolol can be used for hypertension but they are not specific to β1 receptors. They act both on β1 and β2 leading to side effects like bronchospasm, hyperglycemia and even cold sensation.
Selective beta blockers like atenolol, metoprolol, acebutolol and esmolol can be indicated for hypertension and produce less bronchospasm and hyperglycaemia compared with non-selective beta blockers.
Cardiac arrhythmias
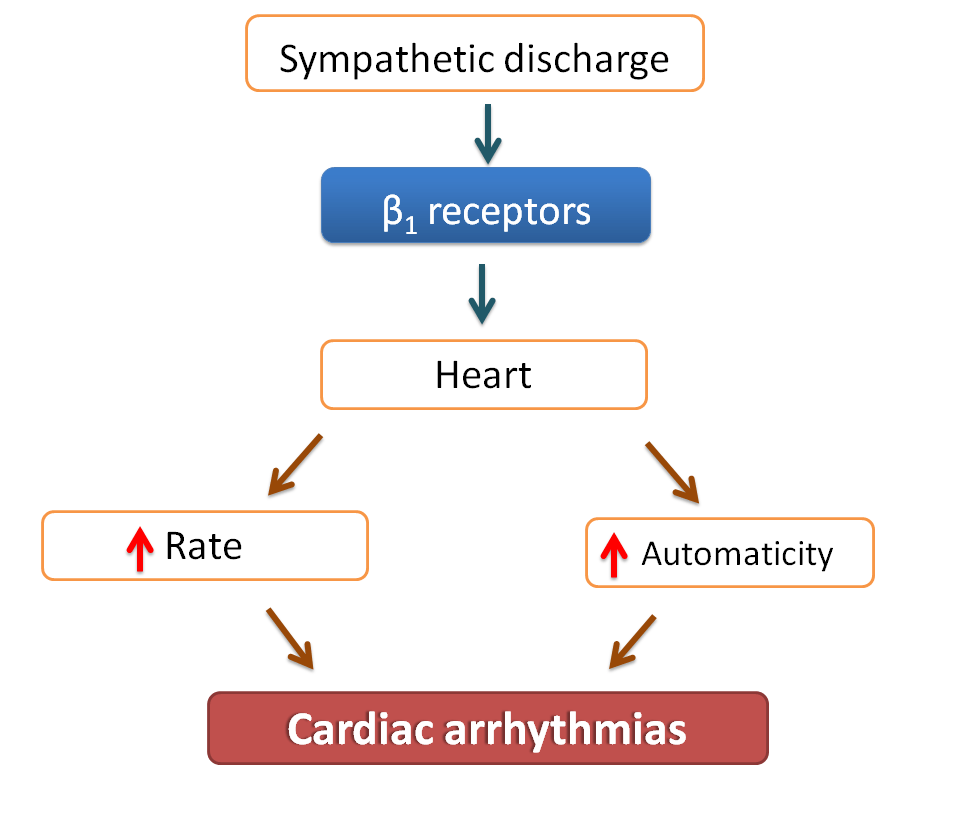
The role of beta blockers in cardiac arrhythmias is a direct one. Beta blockers decrease both heart rate as well as automaticity suppressing any extra heart beats.
They decrease force of contraction and calcium entry in to the cardiac muscle acting on phase II and decrease automaticity by acting on phase 0 of action potentials of the heart.
Heart failure
Elevated sympathetic discharge in heart failure is due to an adaptive mechanism that is improperly controlled and further deteriorating the condition in the heart failure.
In heart failure, a fall in the cardiac output results in decreased renal perfusion pressure stimulating the release of catecholamines. These released catechol amines then act on β1 receptors increasing force of contraction and restore the perfusion pressure.
But this adaptive mechanism may produce a temporary benefit in restoring the condition but increases cardiac work, cardiac oxygen consumption and finally decreases cardiac efficiency.
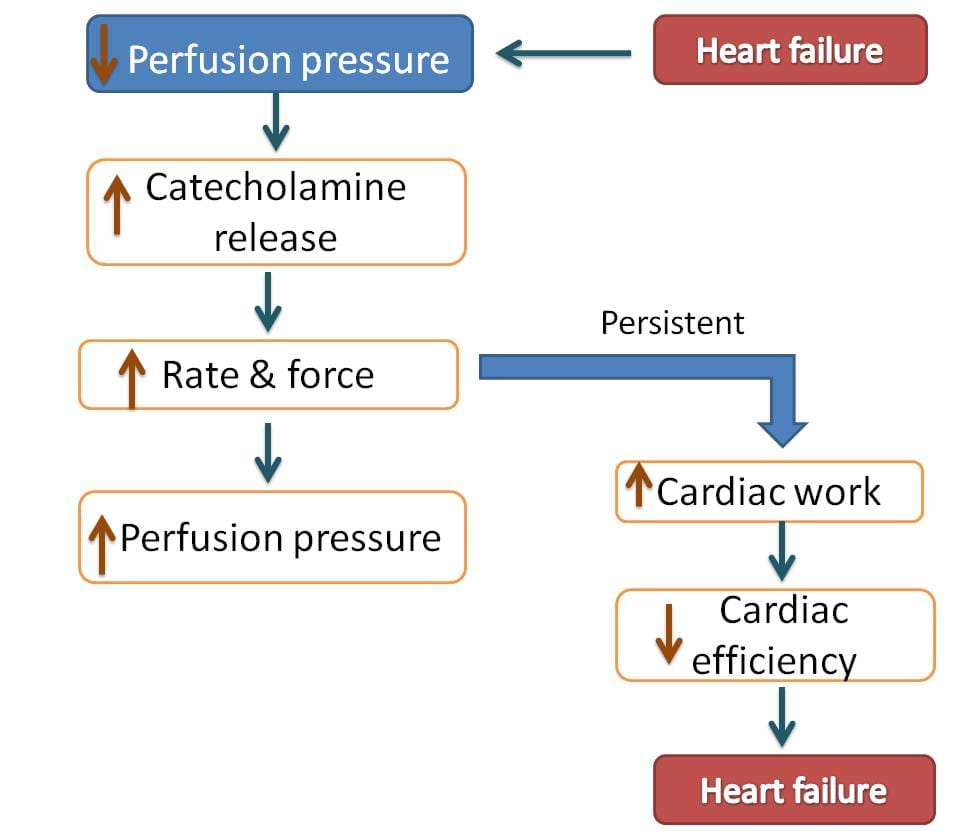
So, beta blockers are used to decrease the cardiac work and to improve the symptoms in heart failure. But all beta blockers are not useful as beta blockers not only decrease cardiac work but also decrease cardiac output which is important in heart failure. Hence beta blockers like metoprolol and atenolol which proved safe with minimal effect on cardiac output are preferred.
Carvedilol is a beta blocker with α-blocking activity which is more advantageous in patients both with heart failure and hypertension.
Angina
Angina is a condition in which pain is produced due to stimulation of nociceptors indicating insufficient cardiac oxygen supply. So, two important goals in angina are either decreasing cardiac work or increasing cardiac oxygen supply. The former can be mediated by again using beta blockers.
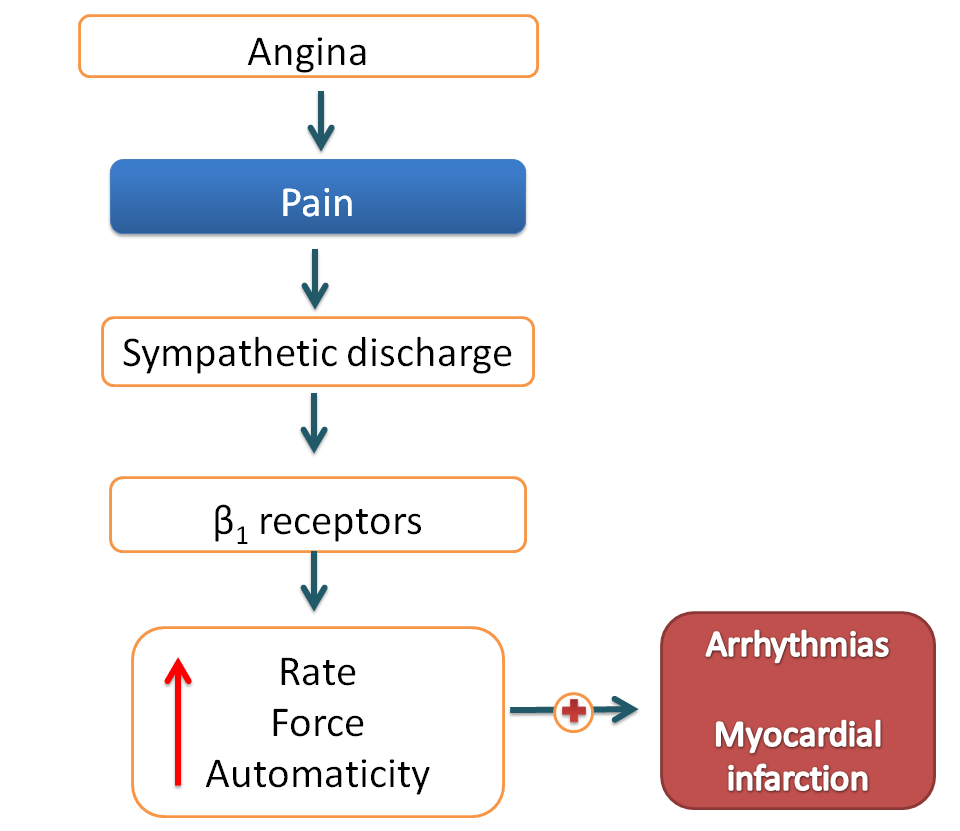
Non-selective beta blockers like propranolol or selective beta blockers like atenolol, metorprolol can be indicated in angina.
Myocardial infarction
Here the role of beta blockers is mostly for maintenance and prevention of further attacks. Myocardial infarction (MI) causes damage of cardiac muscle which results in any of the cardiac disorders just like cardiac arrhythmias or angina. All these are enhanced by further sympathetic activation. So, in this context beta blockers can prevent further deterioration and future attacks of MI.
Anxiety disorders
Anxiety is a condition mainly associated with increased sympathetic activation. This may result in tachycardia, palpitations, tremors and even sometimes sweating. This excess sympathetic stimulation can be inhibited by using non-selective beta blockers like propranolol.
Migraine and Hyperthyroidism
Migraine produces pain which stimulates sympathetic discharge. Similarly, hyperthyroidism can also activate sympathetic discharge. Both of the conditions require beta blockers as prophylactics to prevent further attacks.
In this way, beta blockers play a vital role in majority of the conditions and stand as one group of widely prescribed drugs in medical world.