What is atherosclerosis and how it develops?
by egpat Posted on 08-06-2017
Can you imagine what happens if your blood flow decreases? All your cells get less oxygen, less energy reducing cellular activity finally resulting in cell damage and even cell death. Do you expect any time a tiny plug that blocks your blood vessels can bring all these abnormalities? Yes, its all due to atherosclerosis and its development into heart diseases.
Atherosclerosis is a vascular disease that causes narrowing of blood vessels by formation of dense plug within the inside of blood vessel.
This fibrous plug is called as atheroma. Since it decreases the diameter of blood vessel and hardens the wall of blood vessel it slowly decreases the blood flow.
What causes atherosclerosis?
Well, it is quite clear that atherosclerosis is related to high cholesterol levels in the body. But all people are at same risk? Can’t our body control cholesterol levels?
No, everyone is not at same level in this game.
People with high cholesterol coupled with other risk factors have more chance to develop atherosclerosis than with people having no risk factors.
What are these risk factors?
It’s quite interesting to note that many of the risk factors for atherosclerosis also act as common risk factors for other cardiovascular disorders. So all these are highly interrelated and hence should be strictly controlled.
Any risk factors like hypertension, diabetes, obesity, smoking and family history can initiate or increase the chance of atherosclerosis. Sometimes patients may have multiple risk factors.
How atherosclerosis develops?
Most of these risk factors are associated with various mechanisms like increased after load, generation of free radical and increased oxidative stress all can cause a dysfunction in endothelium which sets the initiation for atherosclerosis.
Can’t we have restore mechanism in our physiological system?
Yes, of course, we have few protective mechanisms which act to restore the condition.
For example any small disturbance in the endothelial dysfunction is corrected by protective mechanisms such as release of nitric oxide which work to improve the blood supply.
Unfortunately in patients with risk factors for atherosclerosis, these protective mechanisms are also not doing well.
In these patients, biosynthesis of nitric oxide is somewhat reduced setting a stage for series of events that finally end to produce atherosclerosis.
Role of LDL cholesterol
Now it’s clear that patients with any risk factors may have chance of developing atherosclerosis if they have raised LDL cholesterol.
Why we are talking about LDL only why not other lipoproteins?
LDL cholesterol generally called as bad cholesterol is really bad in this situation as it involved in pathogenesis of atherosclerosis.
The dysfunctional endothelium attracts monocytes and macrophages and express few of the adhesion molecules which can attach the LDL cholesterol.
Here LDL plays a pathological role. The LDL after uptake into endothelium is oxidised and converted into fatty streaks which are main portion of the atheroma.
As they appear in foam like structure they are called as foam cells.
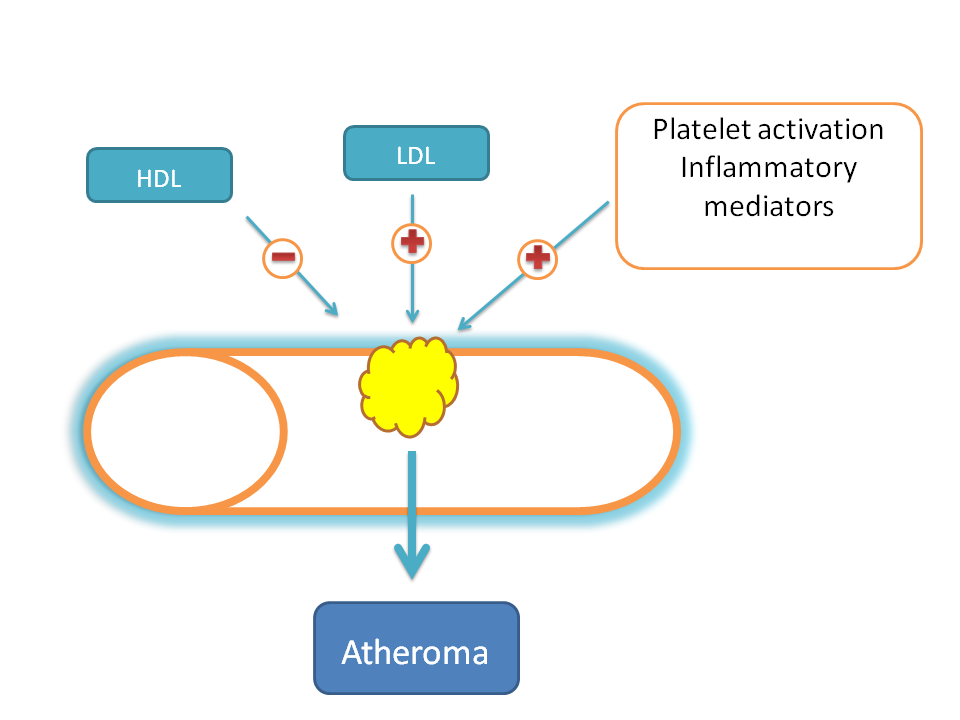
Of course the process of atheroma formation is enhanced by other factors like platelet aggregation, inflammatory mediators which set next stage of inflammation at the site.
This results in further endothelial cell damage and blood coagulation and aggregation of platelets.
Now these foam cells are mixed with cell debris, blood clot, lipids all capped with aggregated platelets to form a fibrous cap.
So, one of the rich components in the atheroma is high lipid content in the form of cholesterol. Here HDL comes into the play.
Cholesterol which is released from tissue damage is carried as HDL cholesterol which is then secreted into the blood.
So some part of the cholesterol can be mobilised into the blood in the form of HDL cholesterol which makes less availability of cholesterol for atherogenesis.
That’s why in contrast to LDL, an increase in HDL levels reduces the risk of atherosclerosis.
Okay, is this atheroma so dangerous? Is it reduces blood flow significantly?
Yes, even though the small reduction in the blood flow is not immediately affecting the functionality but if it is untreated it can be further increased to produce significant obstruction of blood flow.
In addition to this, the atheroma can also be ruptured which brings it to the next stage.
Let’s compare it with our normal physiological mechanism.
What happens if a blood vessel is ruptured and damaged?
Blood is oozes out from the site of damage.
To stop bleeding, blood clotting factors are released forming a fibrin mesh and platelets are activated and aggregated which are then connected by this fibrin mesh to form a clot.
This is great part of physiological system that prevents severe bleeding and loss of blood.
But the same protective mechanism becomes pathological at atheroma.
On rupture of atheroma, these clotting factors are activated forming a mesh coupled with platetelet aggregation forming a dense clot termed as thrombus.
Now this thrombus is somewhat larger in size further reducing the blood flow.
But it is not the end of the story.
This thrombus can be broken into small fragments which flow along with circulation and can block any tiny capillaries.
Now this is alarming. Isn’t it?
When these capillaries are blocked, they can collapse the circulation at the particular target bringing serious effects that can’t be restored easily.
That tiny fragment which makes the situation so serious is termed as embolus.
If embolus blocks cerebral capillaries it may cause stroke, coma or even death in the patient. If it blocks cardiac capillaries it may result in cardiac stroke or heart attack which again increases the risk of the death in the patients.
What is the main goal of atherosclerosis treatment?
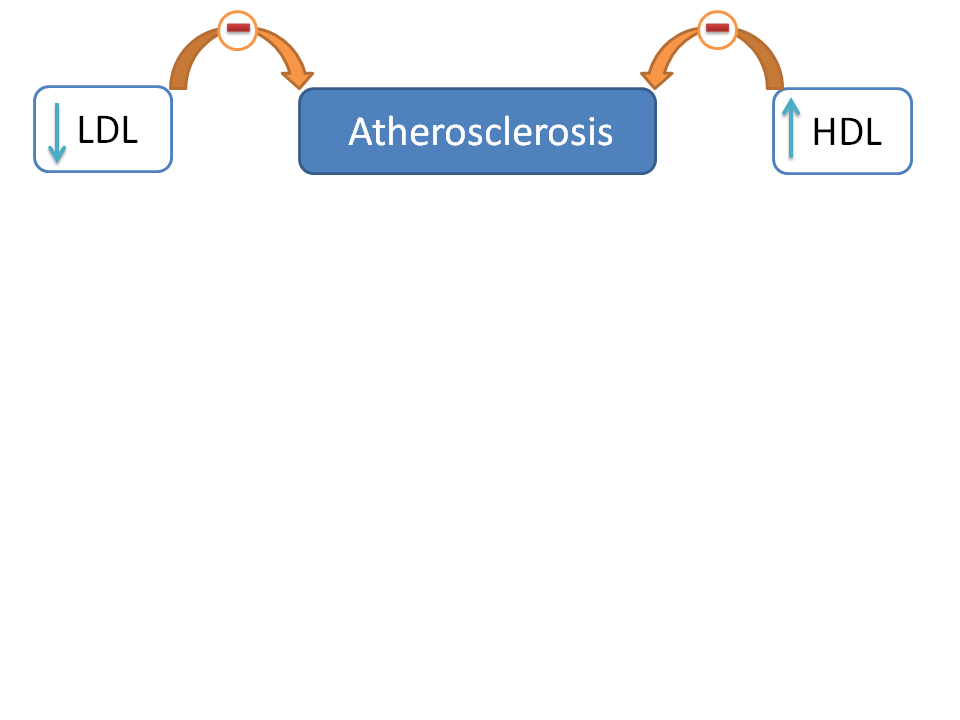
From the above discussion we can clearly conclude that the development of atherosclerosis is closely related with raised levels of LDL and decreased levels of HDL.
So one of the main goals in the treatment is to decrease LDL and increase HDL.
But this is not only sufficient.
Yes, we have to target the underlying cause for atherosclerosis and all the possible risk factors should be minimized.
For example any of the following can bring positive results in therapy by minimizing the risk of developing atherosclerosis
- Regular exercise
- Control of body weight
- Taking fiber rich diet
- Avoiding smoking
- Avoiding alcohol
- Controlling blood pressure
- Control of blood sugar levels
How atherosclerosis is treated?
We have many any cholesterol lowering drugs like statins, fibrates, bile acid binding resins and cholesterol absorption inhibitors.
All the drugs don’t act in similar way in controlling cholesterol levels. For example, statins mainly control LDL-cholesterol whereas fibrates mainly affect VLDL levels.
But among these, LDL-cholesterol plays important role in atherosclerosis. So if we inhibit high LDL cholesterol we can prevent the formation of atheroma. Statins reduce LDL cholesterol significantly by acting as HMG Co-A reductase inhibitors hence treated as drug of choice.
Statins also improve function of endothelium, increase blood supply by formation of new blood vessels and even inhibit platelet aggregation.
On the other hand, fibrates mainly affect VLDL with a minor role on LDL and HDL levels. So they are more preferred in conditions such as in raised triglyceride levels.
Cholesterol lowering medicines other than statins which affect LDL levels significantly include bile acid binging resins like colestipol, cholesyramine and cholesterol absorption inhibitors like ezetimibe.
Will only these drugs occupy the therapy?
No, these drugs are mainly aimed for controlling LDL levels. But according to the condition and stage of the patient few of the drugs can also be prescribed.
For example, antiplatelets like aspirin, clopidogrel can be prescribed in patients with risk of myocardial infarction due to atherosclerosis.
Similarly, anticoagulants like warfarin can also be given to prevent thrombus formation in susceptible patients.
Of course treating with these drugs is not only sufficient instead we have to minimize the underlying risk factors to prevent atherosclerosis.
So patients should be suggested to stop smoking and drinking. Weight should be decreased If patient has any overweight. Diet should be controlled to limit the fatty food intake. Any persistent conditions like hypertension or diabetes should be carefully controlled.
Conclusion
So atherosclerosis is a serious pathological disorder that develops with uncontrolled cholesterol levels and underlying risk factors. A proper management and prevention of atherosclerosis all depends on how cholesterol lowering drugs are used and lifestyle management was established in the patient.